
The partnership you want, the PBM solutions you need.
Schedule a Meeting
Call (612) 672-6500 or 866-718-2845 or complete this form and we’ll follow up.
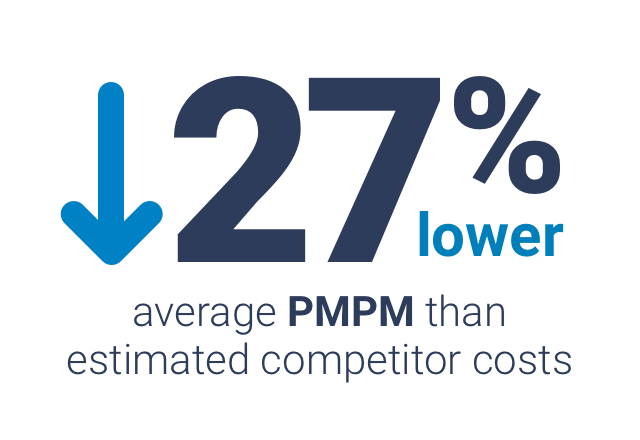
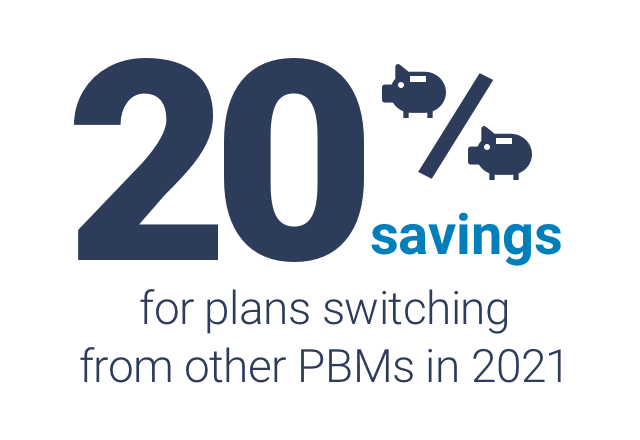
Learn how ClearScript’s PBM solutions will improve your healthcare plan’s pharmacy benefit program with better savings and optimal member health.
"*" indicates required fields
